Welcome back to MND NSW’s Top 5! Over the last 30 days, the MND NSW Info Line has answered hundreds of questions from people living with motor neurone disease (MND), their families, carers, and health professionals.
We have collected the five most common questions we’ve been asked lately. From respite to managing changes to your bladder and bowel function, these are the answers you have been looking for.
Question 1: I am a MND carer, is respite available?
Respite is defined as period of time when someone else takes care of the person you care for. Respite is not just about taking a break from caring, it is also about protecting your health and wellbeing, sustaining your ability to care, and making sure that your loved one is safe.
There are two main types of respite care:
- Emergency Respite is for situations where something unexpected happens such as becoming injured or unwell.
- Planned Respite is for situations where you are not sick or injured but taking a break from caring would be beneficial for your wellbeing.
You can talk to your MND Advisor or call Carer’s Gateway to talk through your respite options. It is also recommended to make an emergency plan so you can feel more prepared for urgent or unexpected situations.
Learn more:
Question 2: I carry the gene for MND, what are the chances that it could be passed down to my children?
Approximately 15% of MND diagnoses are due to a gene change inherited from a parent. This is called Familial MND. There are a number of different genes that have been identified as increasing the likelihood of a person receiving an MND diagnosis. The most common are C9OR72, SOD1, FUS and TDP-43.
If a person knows that they have an MND-related gene, they have a higher likelihood of developing MND. Importantly, it does not mean they will definitely receive a diagnosis with MND.
Couples who are planning to start a family may be concerned about the gene being passed on to their children. If a parent has an MND-related gene, each child has a 50/50 chance of inheriting it.
It is important to speak with your GP or genetic counsellor about your reproductive options or to explore genetic testing.
Learn more:
Question 3: I have noticed changes in my bladder and bowel function, what can I do to manage this?
Some people living with MND may experience changes in their bladder and bowel function. Although MND does not affect the anal sphincter muscles, abdominal muscles may be affected. These muscles are needed to supply the necessary push for a bowel movement. Common causes may include, inactivity, changes in diet, poor fluid intake, or side effects of medications.
Top Tips to manage bladder and bowel changes:
- Optimise fluid intake
- Regular toileting routine
- Equipment such as over-toilet aid, commode, or bathroom rails.
- Medications
- Discuss with health care team including continence nurse, occupational therapist, physiotherapist or dietician.
Learn more:
- Living with motor neurone disease: aspects of care for people with MND, their family and friends
- FlexEquip Product Library: Bathroom
- Maintaining Weight & Nutrition with MND
Question 4: I have just been diagnosed with MND, how do I tell my children or grandchildren?
Having conversations about MND with young people can be difficult. There is no right way or ‘have to’s’ when approaching these conversations. Research shows that young people are better able to cope if they know what is happening and feel okay to ask questions.
Top Tips:
- Use language they can understand
- Be open and honest when replying to questions, even if the answer is ‘I don’t know’
- Talk about what to expect to help them feel less scared of the unknown
- Say MND rather than saying the person is sick or unwell.
Learn more:
Question 5: What is Primary Lateral Sclerosis (PLS) and what are the common symptoms?
MND is umbrella term for a group of diseases that affect the motor neurones. Primary Lateral Sclerosis (PLS) is considered a very rare type of MND. This type of MND on accounts for approximately 3% of diagnoses and can present in similar ways to other types of MND.
Common features of PMA include:
- Muscle spasms and cramps
- Rigid or stiff muscles
- Problems with balance
- Slurring of speech
- Slower progression of symptoms.
Learn more:
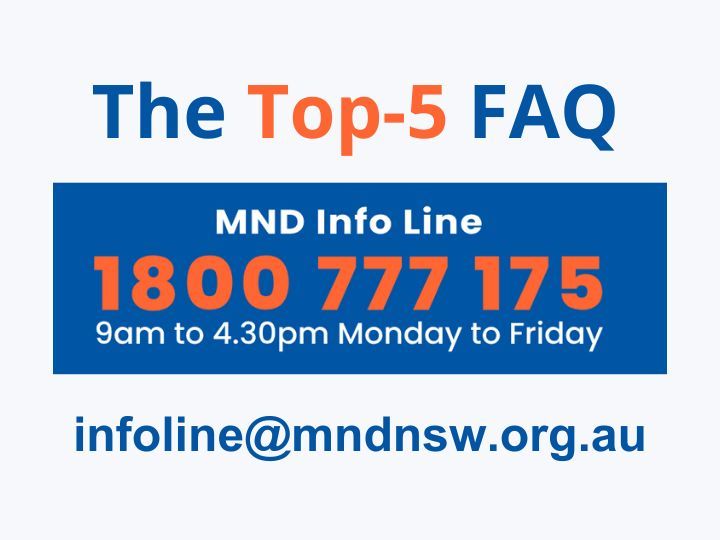
Do you have a question about MND?
Whether you’re newly diagnosed, caring for a loved one, or navigating the MND space as a health professional, we’re here to help.
Call us on 1800 777 175
Or submit and online inquiry at Contact MND NSW
“We can't do this alone. But together, we're unstoppable.”
MND Community Member