My name is John, and I am 65 years young. I was a Soldier for 21 years then a Paramedic for 22 years. I did a lot of contact sports till my early 50s, firstly rugby union, then ju-jitsu. My first symptoms appeared in December 2017 - as I typed, I kept missing keys with my left hand from the loss of fine motor skills.
My GP sent me to a rheumatologist (as there was no local neurologists). The scans and tests showed no brain abnormalities, but some hyper reflexive left arm/hand nerve conduction. As I have a family history of Parkinson’s disease, he could not rule out atypical Parkinson’s, so I was referred to a neurologist who visited nearby. After several visits and more deterioration there was no diagnosis, but he said I didn’t have Parkinson’s. During this time, I retired from work as you can’t be a safe and competent, one-handed Paramedic.
After I moved to Wagga Wagga, COVID hit so it took several months to get to see the local neurologist who referred me to a Sydney based neurologist specializing in movement disorders. By now my entire left arm and hand was weak and uncoordinated and was starting to affect my left leg and speech. Under his care I went to St Vincent’s in Sydney for a battery of tests, was reviewed by an expert panel of neurologists and saw other allied health professionals (speech, physio, social worker). As all my results were unremarkable there was still no diagnosis, but I knew more of what I didn’t have.
In April 2021 I was diagnosed with motor neurone disease. Specifically, upper motor neurone syndrome with some lower motor neurone involvement. It affects the left side of my body, my speech and (unusual for MND) my bladder and bowel awareness.
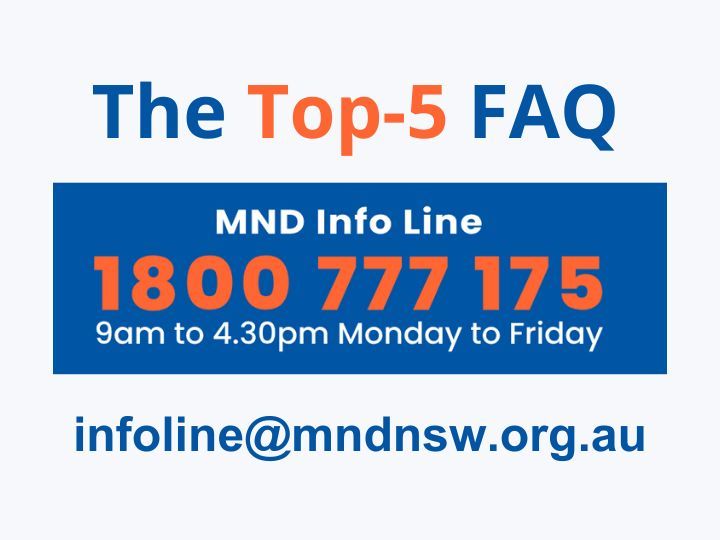
As I was a paramedic, I had a good idea about this disease and its prognosis, but I did more research, and it wasn’t good news. I also contacted MND NSW for disease specific advice. MND NSW were able to link me with another person and we formed our own local support group.
This is my story about how I live with MND. Firstly, I maybe one of the luckier ones whose disease isn’t advancing rapidly, but that isn’t the full picture. Initially before diagnosis I was deteriorating, in Feb 21 a physio described my left hand and arm as unfunctional, I had little arm strength, could not lift it above my shoulder and struggled to hold it against gravity, nor could I effectively grip or hold with that hand.
Mentally I had two choices- die from MND or live with it. A psychologist helped turn my negative thoughts (dying) into a positive (living with). It is unfortunate that the science of MND strongly directs one's thoughts to the negative, but it would be wrong to ignore those statistics, data and facts and live in denial or false hope. This is a terrible disease that can quickly kill and can be devastating news for the person, their family, and friends.
To help anyone newly diagnosed, or anyone uncertain, I share my journey and offer this advice. If under 65 (as in my case), get accepted by the NDIS and find a good support coordinator and plan manager. I asked my therapists, and the NDIS provided me with a list of local agencies. I called or visited all of them and then decided who would be the best fit for me. Getting into the NDIS and getting a good plan will pay for your support workers, assistive technology, and your therapists (but not your doctors, alas).
Find a senior GP with preferably some neurological experience (don’t be afraid to look around till you find one you can work with and has the capacity to care for you). The GP will tie together your needs like referrals, scripts, tests/results, reports (NDIS, Transport NSW, Taxi Transport Subsidy Scheme and Application for Transport and Travel for regional/rural patients to go to Sydney for specialist tests and care). Your GP will monitor your physical health, wellbeing, resilience, and mental health as it is important not to neglect these and be solely focused on MND.
Get referred to a neurologist who knows of the latest research and trials. I needed a neurologist's report for the NDIS to accept me (I saw several until I was referred to my current doctor, but that is how our health system sometimes works - be patient). Your neurologist will be the key to charting your journey with MND and advising others. As no two of us have the same journey, this personalized reporting will aid others to tailor their care or support to your needs. My neurologist visits Wagga 3 monthly, she thinks I am doing amazing and has encouraged me to share my story.
Get referred to a Respiratory Specialist to monitor your breathing and look for signs of respiratory failure and to keep track of any changes and prescribe appropriate therapies. For me this is a BIPAP machine for use at night.
Get referred to a Pain Management Doctor/Specialist (therapies and/or medicine to manage muscle spasticity pain) and a Rehabilitation Doctor to link into allied health and for supporting evidence for their need, as these will increase and/or change over time.
For Allied Health, find an experienced and cooperative physiotherapist, an occupational therapist, an exercise physiologist, a speech pathologist, a podiatrist and a myotherapist (advanced remedial massage). I also have a hand occupational therapist, a specialist hand physiotherapist, a social worker, and a dietician.
As my bladder and bowel awareness is affected, I have a urologist and a continence specialist/nurse. Earlier I had psychologist support, but I no longer require this, though others may find it beneficial for longer.
Why do I make these suggestions? Without my team and my determination, I believe I would have continued to rapidly decline. As I near the 2 years since diagnosis and 5 years since symptoms appeared, I am holding some aspects of MND at bay and can even make some progress. Through physiotherapy, hydrotherapy, exercise physiology, hand therapies and myotherapy I can lift my left arm above my shoulder, have almost full range of motion, improved strength, less swelling and better lymph return due to reduced spasticity and improved muscle tone. I can use my left hand to grip and hold, it is not 100% but it’s a vast improvement on ‘unfunctional’. Exercise and speech pathology have reduced episodes of saliva penetration and my swallowing is good with no diet restrictions. My respiratory function is stable, as my respiratory doctor quickly diagnosed sleep apnea due to early respiratory muscle failure secondary to MND. Exercise has helped maintain my respiratory function/endurance and this has allowed me to be able to still speak. I do various speech exercises and train with my speech pathologist regularly.
On a personal level, and for future proofing, I have made a will, power of attorney, enduring guardianship and advanced care directive and my family know how to access these, what they are for and what they contain. I wrote a letter to them detailing my finances (banking, shares, tax file number, super, usernames and passwords, and instructions to finalize and close accounts and subscriptions). I am an organ donor, so they needed to know this. Through my rehab doctor and social worker, I have visited the local nursing home/hospice and I know I will be well cared for and comfortable when my end of life comes. When that happens, I have made my wishes known to my children including donating my adaptive technology to benefit other people living with MND.
Be prepared for major lifestyle changes. Initially, I changed my license to a restricted one (and let my insurance know) and got a disabled parking permit. Once I no longer felt safe driving, I voluntarily surrendered my license and am now dependent on wheelchair taxis. After a bad fall in May I started using a powered wheelchair for fatigue mitigation and falls prevention. I can still walk with a 4-wheel walker, going from less than 20 steps a day to hundreds and have had no further falls. I have an electronic bed for sleep positioning and to help get in and out and a lift chair for sit to stand. As I live alone, I have a morning support 5 days a week (falls monitoring from bed to toilet to shower, and to assist with some dressing). I have my lawn and gardening done and afternoon domestic support (cleaning, laundry, some pet care, and a welfare check).
What has been hard? Telling my family and friends (MND NSW information/support helped immensely with my young teenage son, who struggles with his dad being sick). Although I am immensely grateful for the NDIS, and my plan gives me the support and therapies I need, I do find the system too slow and bureaucratic for someone with MND because by the time you get your plan, support, or equipment your needs may be changing and this at times is more stressful than living with this disease.
What has been easy? Working with great doctors, health professionals, support workers/coordinators, plan managers and adaptive technology providers. All have been kind and caring and many are now friends. Keeping my mind alert in a declining body is very important, most of my hobbies I can no longer do but I still enjoy computer games and use commercially available tech to help me game.
Accept that good days will be OK and be thankful for them and celebrate every moment of joy and love. Laugh when you can. On the other hand, accept that bad days will be really, really bad. Don’t be afraid to cry when sad and overwhelmed. Listen to your body to manage your fatigue as best you can and accept the help of others.
With hard work and determination, and the right support and therapies I have regained some function or slowed aspects of MND. It isn’t easy, it’s like a full-time job, out every day doing activities/seeing therapists and some days I just don’t feel I up to it, but doing it strengthens my self-worth, resilience, and determination. It’s not a cure, nor am I likely to be cured and I am very much aware that my MND progresses, and I continue to deteriorate! My next major challenge will be to confront the changes and communication barriers when I can no longer speak.
I hope that my story can guide or inspire, but I do not wish to cause distress to those who have lost someone or to those who may not be able to use it. I encourage everyone with MND to tell their own story to inform and assist others who live with us or care for us. I tell mine because in the words of one of my therapists who has seen my journey –
“… you really should be the pinup boy for motor neurone disease, please tell your story …”